Plasmapheresis
In Dr. Anil Patel’s kidney clinic, plasmapheresis is likely utilized as a therapeutic intervention for various kidney-related conditions, autoimmune diseases, and other systemic disorders. Here’s how plasmapheresis might be implemented and managed in his clinic:
Patient Selection and Evaluation: Patients who may benefit from plasmapheresis undergo thorough evaluation by Dr. Patel and his team. This assessment includes a detailed medical history, physical examination, laboratory tests, and imaging studies to diagnose the underlying condition and determine the appropriateness of plasmapheresis as a treatment option.
Treatment Planning: Based on the patient’s diagnosis and clinical condition, Dr. Patel develops an individualized treatment plan that includes the frequency, duration, and modality of plasmapheresis. This plan may involve a series of plasmapheresis sessions over several days or weeks, depending on the patient’s response to therapy.
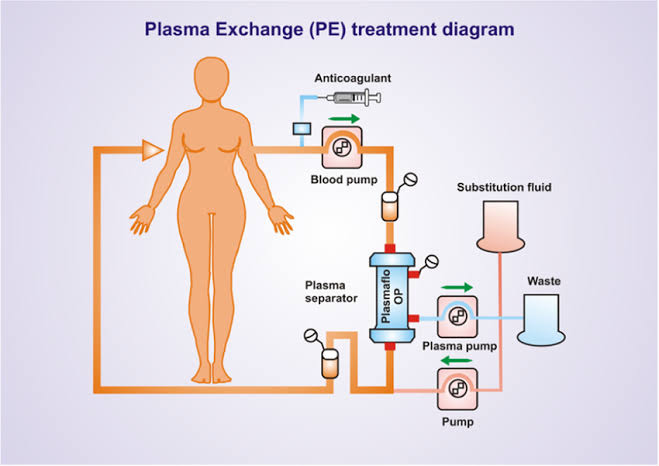
Vascular Access Placement: Dr. Patel ensures appropriate vascular access for plasmapheresis by placing a central venous catheter (CVC) or other vascular access device. This allows for the withdrawal, processing, and return of blood during the plasmapheresis procedure.
Plasmapheresis Procedure: During plasmapheresis sessions, blood is withdrawn from the patient through the vascular access device and passed through a plasma separator or centrifuge to separate plasma from cellular components. The plasma, which contains harmful antibodies, immune complexes, or other pathogenic substances, is removed and discarded, while the cellular components are returned to the patient’s circulation.
Replacement Fluids: To maintain blood volume and prevent hypotension during plasmapheresis, Dr. Patel administers replacement fluids, such as albumin or saline solution, to the patient as needed. Careful monitoring of fluid balance and hemodynamic status is essential throughout the procedure.
Monitoring and Supportive Care: Dr. Patel and his team monitor patients closely during plasmapheresis sessions, assessing vital signs, fluid status, electrolyte levels, and other relevant parameters. They provide supportive care, such as hemodynamic support, electrolyte replacement, and symptomatic management, as needed to ensure patient safety and comfort.
Response Assessment: Following plasmapheresis treatment, Dr. Patel evaluates the patient’s response to therapy, monitoring clinical and laboratory parameters to assess improvement in symptoms, disease activity, and overall outcomes. Additional plasmapheresis sessions may be scheduled based on the patient’s response and treatment goals.
Patient Education and Counseling: Dr. Patel educates patients and their families about the purpose of plasmapheresis, the treatment process, potential risks and benefits, and what to expect during therapy. Clear communication and patient education help alleviate anxiety and promote active participation in care.
Multidisciplinary Collaboration: Plasmapheresis often involves collaboration among various healthcare professionals, including nephrologists, immunologists, hematologists, and transfusion medicine specialists. Dr. Patel coordinates care with these team members to ensure comprehensive management and optimal outcomes for patients undergoing plasmapheresis.
Overall, plasmapheresis is an important therapeutic modality in Dr. Anil Patel’s kidney clinic for treating a variety of kidney-related and systemic disorders, with a focus on personalized care, close monitoring, and multidisciplinary collaboration to achieve the best possible outcomes for patients.